About 30 years ago, the American Board of Obstetrics and Gynecology approved three new subspecialties in the field of obstetrics and gynecology. These subspecialties were gynecologic oncology (women’s cancer), perinatology (high-risk pregnancies), and reproductive endocrinology (infertility and other reproductive hormones). It was the hope when these subspecialties were developed that they would advance those three areas of women’s health.
As one looks back on the development of the reproductive endocrinology training programs, they originally started with the emphasis on pelvic surgery. However, in 1978, when the first baby was born by in vitro fertilization (IVF), the specialty changed dramatically. Its focus, over the last 12 years, has been on the development of the skills needed for IVF. As a result, many younger reproductive endocrinologists do not, at this time, have the surgical skills necessary to do some basic and most advanced reconstructive pelvic surgeries.
Over a decade ago, the Society of Reproductive Surgeons, a group within the American Society of Reproductive Medicine, began to recognize this deficiency and foster the development of postgraduate fellowship programs which would have, as one of their major emphases, training in pelvic surgery, microsurgery, laser surgical applications, and so forth. These training programs have grown slowly over the past 10 years, but it is in this area that Surgical NaProTECHNOLOGY has its major focus.
Surgical NaProTECHNOLOGY is a specialized form of gynecologic surgery whose primary aim is to reconstruct the uterus, fallopian tubes and ovaries in such a way that pelvic adhesive disease can be eliminated and not caused by the surgical procedure itself. It is, in a sense, a “near-adhesion free” form of surgery.
“Near-Contact” Laparoscopy
Diagnostic laparoscopy is a technique which is not universally well taught in the training programs of obstetrics and gynecology. Often, laparoscopic technique is learned by the young physician as they undergo laparoscopic sterilization procedures. However, the use of the laparoscope for the use of diagnostic purposes is actually significantly more complex.
One of the techniques that is important in doing good diagnostic laparoscopy is something that is referred to as “near-contact” laparoscopy. In this situation, the laparoscope must be brought in close contact with the tissues in order to actually see what is going on. A good example of this is shown in Figures 65-25 through 65-27. In the upper photograph, the uterus, tubes and ovaries are observed and there are two small defects observed on each side of the uterus. In the next photograph, a closer view of one of the defects is seen but one could miss the endometriosis that is present on this view. In the third view, however, the laparoscope is brought right in contact with the opening of that defect and the dark red area in the background is endometriosis. It becomes quite visible when the laparoscope is placed close to the tissues. “Near-contact” laparoscopy is a fundamental technique of Surgical NaProTECHNOLOGY.

Excising Endometriosis
Surgical removal of endometriosis carries with it the best chance for success, both in terms of pain relief and in subsequent pregnancies. However, if the surgeon is not adequately trained to be able to provide a good surgical approach which will remove the endometriosis while preventing subsequent adhesions, the chances for success are quite limited.
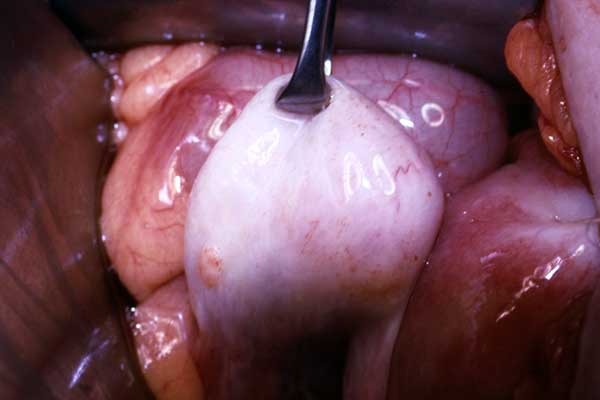
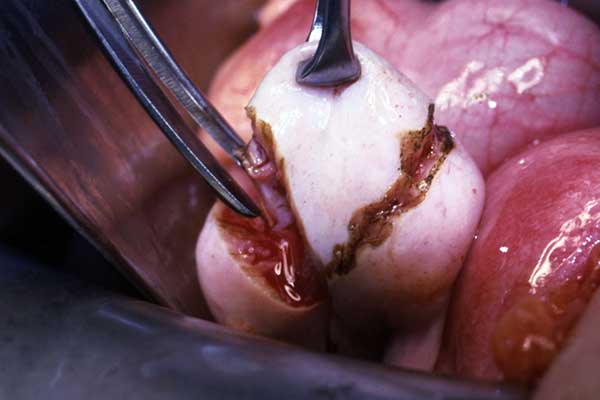
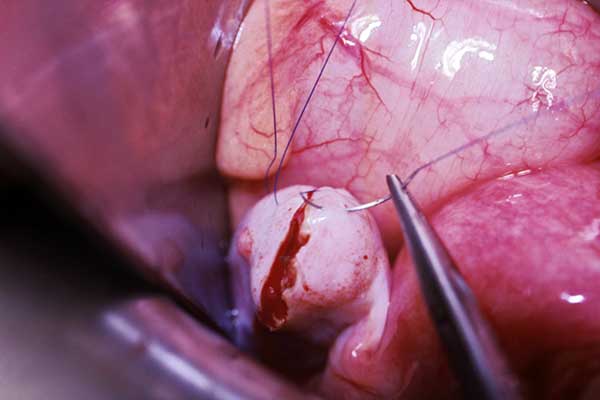
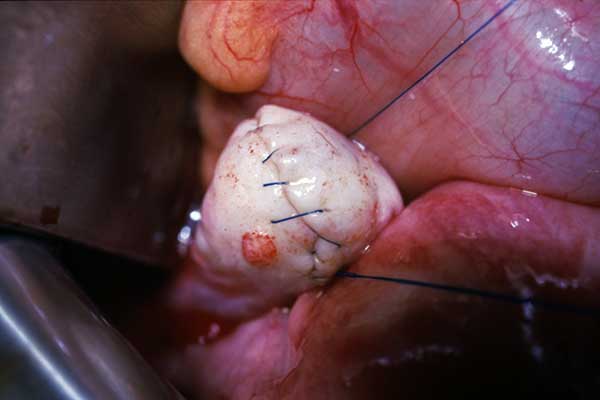
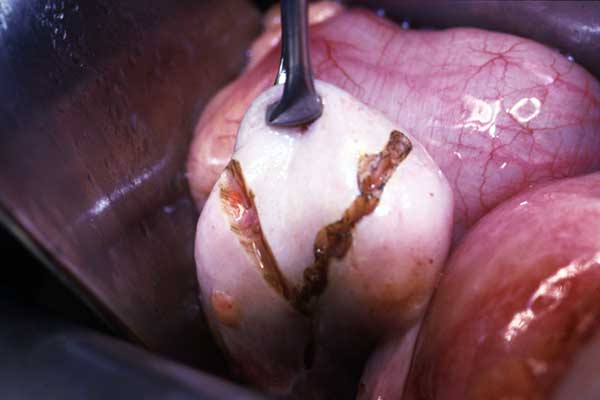
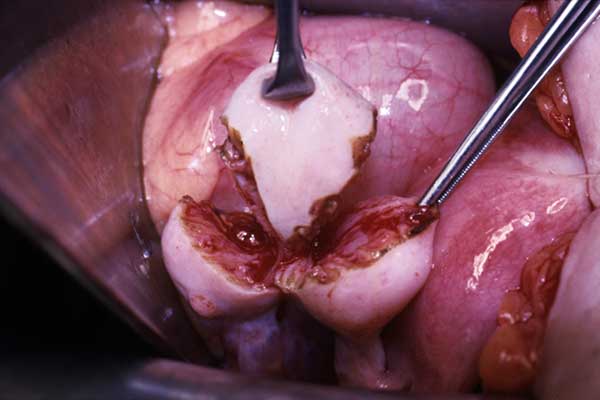
In Figures 70-1 through 70-5, an area of endometriosis on the front portion of the uterus is excised and it is repaired using a suture called Prolene. The Prolene suture is a permanent suture which is very non-reactive. In addition, the superficial tissues are inverted inwards so that, at the conclusion of the procedure, one has a surgical closure which is smooth, glistening, there is no abrasive tissue present, and the suture itself is completely nonreactive. This is illustrated best in Figure 70-5.
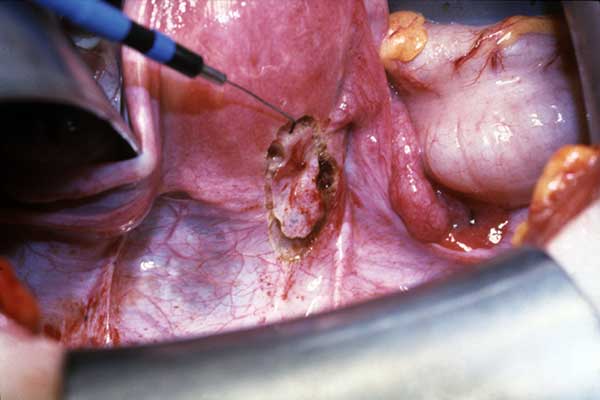
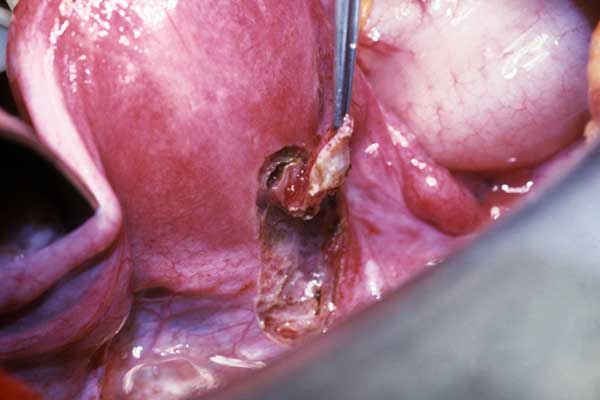

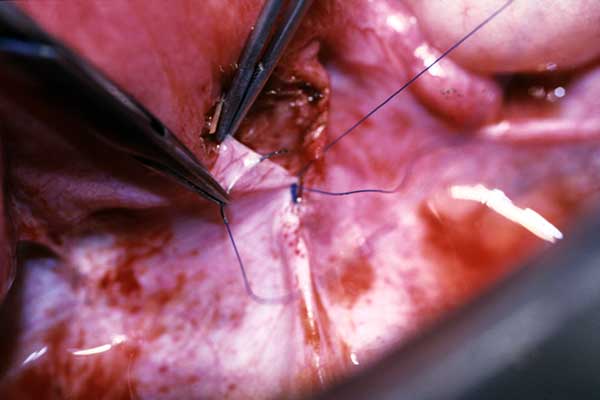
Figures 70-1 through 70-5, p 952 from the NaPro textbook. In this example of endometriosis on the anterior uterus and posterior bladder, an incision is made around the area of endometriosis into the peritoneum using a microcautery. The endometriosis is excised and the peritoneum is repaired using a 4-0 Prolene, running imbricating suture leaving a smooth glistening peritoneum exposed.
Wedge Resection for Polycystic Ovaries
Women who have polycystic ovarian disease, have very large ovaries which have multiple cysts within them. They do not function very well and their menstrual cycles are long and irregular. They do not ovulate on a regular basis, thus, infertility is quite common in this situation.
In 1950, the pregnancy rate following ovarian wedge resection was 66 percent.
However, when Clomid was introduced in the mid 1960s, the pregnancy rate was only about 30 percent, but everyone got the impression that it was a better form of treatment and the medical profession adopted it. More recently, using in vitro fertilization techniques, the pregnancy rate is only 23 percent and there is continued emphasis on this being an even better treatment.
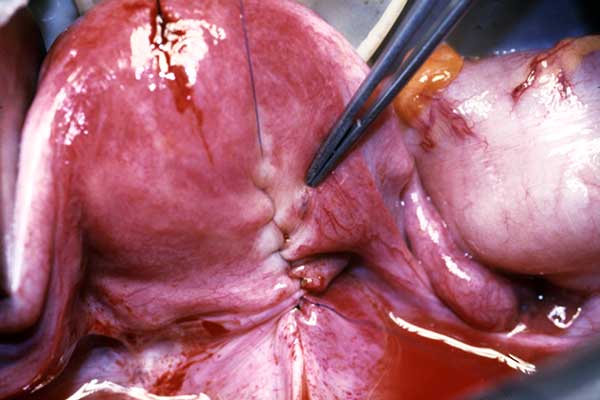
Much of this occurred as a result of surgical techniques which were used for the ovarian wedge resection and caused a large number of pelvic adhesions. However, this has been completely eliminated with the use of Surgical NaProTECHNOLOGY techniques. The technique used for ovarian wedge resection is illustrated in Figures 75-3 through 75-7 and 75-8 through 75-11. Here, an incision is made into the ovary using a carbon dioxide laser. The wedge of tissue is removed and the ovary is repaired using the Prolene suture once again and inverting the edges. When the final result occurs, as illustrated in Figure 75-11, this results in excellent healing and no adhesions.

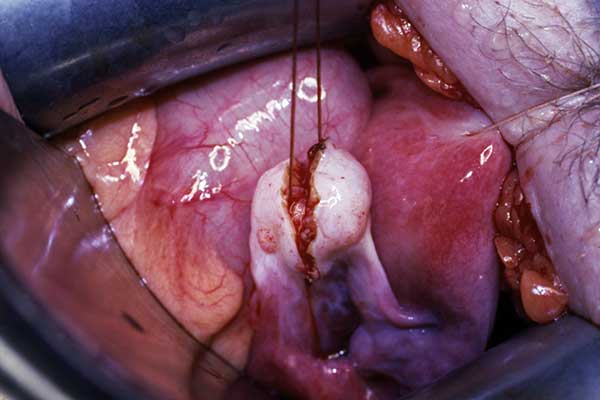
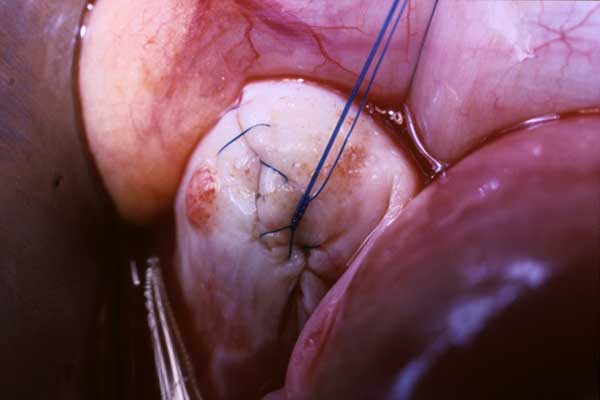
Figures 75-3 through 7-11, pp 1025-1026 from the NaPro textbook. Steps in an ovarian wedge resection performed on a polycystic ovary.
Preventing Adhesions
The prevention of adhesions at the time of surgery involves multiple surgical steps. These are explained in detail in the Medical and Surgical NaProTECHNOLOGY. While these techniques were evolving over a period of 20 years, there was a remarkable decrease in the formation of adhesions with utilization of these techniques. This is summarized in Figure 81-1 which shows the historical advancement of the prevention of postoperative adhesions with the use of Surgical NaProTECHNOLOGY techniques. What is most noteworthy is the decline in the total adhesion score from 33.3 to 6.0 in the period of time from 1994 through 2004. This was a significant improvement over the previous 10 years where the reduction in adhesion scores went only from 33.8 to 18.1.
A description of how this is all accomplished cannot be adequately conducted with this description of Surgical NaProTECHNOLOGY. One is definitely referred to the textbook on The Medical & Surgical Practice of NaProTECHNOLOGY.Back to Top
Selective Hysterosalpingography
In evaluating infertility, it is common to perform hysterosalpingography (HSG). The HSG has become a normal part of the routine infertility evaluation. While this test of tubal integrity and study of the intrauterine cavity represents a significant improvement over previous tests, it has continued to have shortcomings. Perhaps one of the most difficult aspects of the infertility evaluation is to study the anatomic and functional integrity of the fallopian tubes.
Beginning in 1966, efforts were made to evaluate the fallopian tubes selectively using fluoroscopy and contrast material. This procedure subsequently became known as selective hysterosalpingography (SHSG). A number of investigators have also added to the procedure various aspects of transcervical catheterization of the fallopian tubes (TCFT). It has also been suggested that tubal perfusion pressures could provide important diagnostic information and further investigation of this area was encouraged. In 1999, Hilgers and Yeung described a group of patients for whom the intratubal pressure (ITP), at the time of the SHSG, was obtained before and after TCFT. This procedure is shown in Figures 66-7 and 66-8.

This technique will allow the physician to identify partially obstructed fallopian tubes because of an elevated pressure. This is usually caused by debris that forms within the fallopian tube. It can be dislodged and cleared with the placement of a flexible-tip metal guidewire all the way down the fallopian tube. After such a procedure is performed, the pressure is generally normalized.
In addition, by placing the flexible guidewire, a complete obstruction and/or an organic obstruction can also be differentiated from these more functional obstructions. This is an important advance in the field of reproductive medicine because it identifies those who might be good candidates for reimplantation of the fallopian tubes, thus making them patent again.
